My Mental Health Practice History 1960s - 2020s
I began my Mental Health Practice History as a counselor and educator in 1968 in the drug abuse field. My professional practice experience includes: 1) community organization, 2) program development, 3) proposal writing, 4) fundraising, 5) child abuse investigation, 6) child welfare, 7) clinical diagnosis and treatment, 8) family reunification, 9) child custody evaluation, 10) custody mediation, 11) curriculum development, 12) education, 13) forensic analysis, 14) expert testimony and 15) clinical supervisor. I have presented numerous papers on subjects related to my Mental Health Practice History such as, parenting, communication, family dynamics, clinical skills, and education for your mental health.

My Mental Health Practice History would never have happened without my Troubled Beginnings from adverse childhood experiences. I was a victim of child abuse that began in early childhood and continued into my preteen years. I acted out My Troubled Beginnings as a vandal and graduated to juvenile delinquency and drug addiction by middle school. Arrests, juvenile hall, probation, dropping out of high school, and psychiatric hospitalization eventually led to placement in Topic House, a residential treatment center.
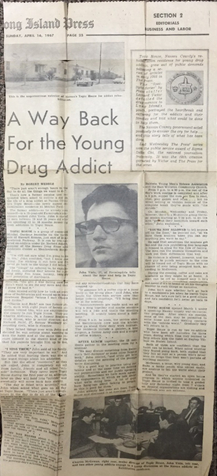
Topic House opened with eight original residents. As one of the original eight residents, I was often selected to tell my story to community groups & organizations on Long Island and New York City. News stories followed, and so did radio interviews and TV appearances. I left Topic House in August of 1967, married that November, and had three children by May 1971.
My Mental Health Practice History probably began in January 1968 when my probation officer invited me to organize and co-lead a group with his teenage probationers—kids whose Troubled Beginnings included drug abuse. Indeed, I stepped into a career as a Counselor & Educator.
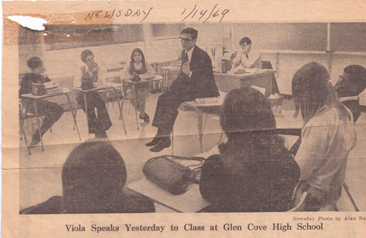
My Mental Health Practice History became legitimized in January 1969 when courageous administrators and board members of the Glen Cove School District became the first public school in the country to hire an ex-drug addict as a Counselor & Educator. Equipped with my Troubled Beginnings and high school equivalency diploma, I taught junior and senior high school students drug abuse prevention. I developed an in-school counseling program for students who sought help for their substance abuse problems.
My interest in psychoanalytic literature helped to quell my imposter anxiety. A wave of expectations, responsibilities, publicity, and controversy quickly accompanied this step in my Mental Health Practice History. I began my college education while developing programs that guided teenagers toward sobriety, prevented others from developing drug problems, and helped parents recover from the fear, anger, and helplessness that crippled communication with their teenagers. Undeniably, the community of Glen Cove created a path for the Mental Health Practices of many ex-drug addicts and later recovering alcoholics counselors who followed me into schools and community-based agencies in the 1970s.
As the summer of 1969 approached, the students practicing sobriety needed counseling services to continue. The students' needs challenged my Mental Health Practice. Thus, I learned about Community Organization and Program Development on the Job. I organized a group of community leaders that supported my work in the schools to form H.E.L.P., Inc. (Honesty and Education Leading to Prevention), a community-based non-profit counseling agency. I directed H.E.L.P., Inc. through the 69/70 school year while continuing my duties with Glen Cove Schools. I co-founded the New York State Joint Coalition of Community Services that year. The Joint Coalition, composed of new state-wide non-profit substance abuse agencies, lobbied and received an annual $20,000,000 allocation from the NY State Legislature. I served as president for that first year and two years as treasurer and remained a consultant to Governor Nelson Rockefeller. My Mental Health Practice History was learning Policy Development and Political Organizing. The work of the Joint Coalition and the state funding for community-based substance abuse programs drew news media and public attention. Public speaking, lecture requests, and media interviews became frequent. My Mental Health Practice skills became sharpened as a Public Speaker and Guest Lecturer.
In the summer of 1970, I was recruited by Port Washington, a neighbor community west of Glen Cove, to develop a community-based substance abuse counseling and education program. Using my Mental Health Practice skills, I guided community leaders and school administrators to form Port Alert, Inc. I developed the clinical modality, a community outreach, and an education program for the Port Washington Public Schools. I coordinated with community organizations and hired counselors. I authored a grant that was funded by the Nassau County Drug and Alcohol Commission (that later became the County's Department of Drug and Alcohol Addiction). By now, my Mental Health Practice History has grown to include Administrative skills.
While developing Port Alert, Inc. (still providing service as Port Counseling Center in the exact location), I was recruited by Long Island Jewish Hospital (LIJ) to consult on a grant proposal submitted to the Federal Department of Health Education and Welfare (HEW). HEW responded favorably but was concerned about LIJ's proposal to develop a multimodality substance abuse treatment facility in Queens General Hospital (QGH). I informed LIJ that the program lacked vital service components and staffing patterns that would not meet the needs of the culturally diverse communities of central and southeastern Queens. My Mental Health Practice History now includes Policy and Program Analysis and Consultation. LIJ hired me as a consultant to rewrite the proposal, then later hired me to implement and administer the program when the funding was assured. I began building a staff of 60 as Para-professional counselors and coordinated the Multimodality Treatment Program with the professional and nursing staff provided by LIJ and Mary Immaculate Hospital, respectively. My arrangement with LIJ included completing my commitment to Port Alert, Inc. until I assisted the board of directors n hiring a new Executive Director. Subsequently, I joined the LIJ staff full-time to build this complex hospital-based treatment program. Indeed, my Mental Health Practice History was now expanding into Hospital Administration.

was a pulmonary facility opened in 1935,
later converted to a New York City General Hospital.

was a pulmonary facility opened in 1935,
later converted to a New York City General Hospital.
The Queens General Hospital Multimodality Substance Abuse Treatment Program became operational by the end of 1971. Each of the six treatment units opened when staff and facility requirements were met. These units included: 1) In-Patient Detoxification, 2) In-Patient Treatment Center, 3) Out-Patient After Care, 4) Out-Patient Counseling Center, 5) Community Outreach, and 6) Prevention & Education program. The Queens Hospital program integrated paraprofessionals (formerly ex-addict counselors) and professionals in Medicine, Nursing, and Psychology with a Twelve-step philosophy.
In the winter of 1972, Queens General Hospital’s programs were mainly operational. Patients and community members were receiving service. I received a distressing call from Port Alert's Board President; he informed me their Executive Director, my replacement, passed away suddenly. The board authorized the president to inquire if I would return to my former position with Port Alert. A plan was developed to transition the management of the Queens Hospital programs to Long Island Jewish Hospital's Social Work Department. Over the next several months, I wore two hats and eventually returned as full-time Executive Director of Port Alert, Inc. In 1975 I resigned from Port Alert to complete my professional education. From 1968 to 1975, my Mental Health Practice History gained skills in administration, business management, clinical practice, community organization, consultation, education, fundraising, program development, personnel management, proposal and grant writing, research, and supervision. I continued my appointed positions on the NYC Mayor’s Council on Drug Abuse, the NY State Council of Youth Service Agencies, and the Nassau County Mental Health Board while attending universalist full-time.
The 1970s were a whirlwind decade for my education, family, and professional development. Two of three children were born in 70 and 71. I authored, defended, and earned a Bachelor of Science (BS) Degree in Drug and Alcohol Abuse and Human Behavior from the State University of New York. I also earned a Master Social Work (MSW) Degree from Adelphi University School of Social Work. As a preteen, I read a biography of Sr. Isaac Newton and was moved by his famous quote: “If I have seen further than other men, it is because I have stood upon the shoulders of giants.” Indeed, this quote has continued to be the brand of my Mental Health Practice History. During the decade, I climbed upon the shoulders of giants and read the collected works of Sigmund Freud and Carl Jung and studied Melanie Klein, John Bowlby, Anna Freud, Mary Main, Mary Ainsworth, Erik Erikson, Alfred Adler, Fritz Perls, Wilhelm Reich, Otto Kernberg, R.D. Lang, Harry Stack Sullivan, Emile Durkheim, Ralph Linton, George Herbert Mead, and Max Siporon.
In 1977 I was hired by the Nassau County Department of Drug and Alcohol Addiction to provide administrative and staff development consultation to community agencies funded by the department and provide clinical services at the East Meadow Community Counseling Center. I earned a Graduate Assistant position at Adelphi University School of Social Work. I wrote grants and developed field placement training programs for MSW students to serve underprivileged and disabled populations. The university received millions of dollars from the Federal Department of Health Education and Welfare to develop programs to train social work students to serve disadvantaged people. During my graduate assistantship, my Mental Health Practice History became enriched with sharper writing, curriculum development, instruction, program development, and community organizing skills.
When I completed my MSW degree, I was hired by Adelphi University as Assistant Director for Off-Campus Social Work Education and Continuing Education Programs for professionals. I also taught Administration of Social Welfare Agencies to graduate students. While employed at Adelphi, I established an off-campus MSW program on Staten Island. I revised intake and administrative procedures for all off-campus social work programs in upstate NY, the Virgin Islands, and the Long Island Rail Road. I also developed and produced several continuing education programs for social work professionals. My Mental Health Practice History gained additional and valuable experience in university administration and graduate and professional education.
In 1980 I traveled with my family across the United States and relocated to the Morongo Basin, located at the southeast corner of the Mojave Desert in Southern California. This area often called the high desert (altitude range from 2000 to 6000 feet), is the easternmost exurban region of San Bernardino County. Yucca Valley, our home, is 125 miles east of Los Angles and 35 miles northeast, and 3000 feet higher than Palm Springs. The Morongo Basin is also the home of the Joshua Tree National Park and the neighboring communities of Joshua Tree, Twentynine Palms, Yucca Valley, Morongo Valley, Landers, and Wonder Valley. The world's largest Marine Corps Base and the only place in the US where our military uses live ammunition during training is also in the Morongo Basin.
The Marine Corps Air Ground Combat Center is known to locals and the military as MCAGCC (pronounced MaCackcee). In 1980 the Morongo Basin was sparsely populated. There was no local government or court, and the nearest county mental health clinic was 70 miles from Yucca Valley in San Bernardino. In September 1980, I was hired as a therapist by the Morongo Basin Counseling Center (MBCC), a non-profit agency with offices in Yucca Valley and Twentynine Palms. MBCC Functioned as an unofficial satellite clinic of San Bernardino County’s Department of Mental Health. I had considerable difficulty adjusting to MBCC’s lack of treatment protocols, resources, and psychiatric coverage. I felt I had traveled back 50 years, and my Mental Health Practice History entered the dust bowl of the 1930s. Within a few months, I knew I could not continue working for this agency, but my options were limited.
In December 1981, I worked as a Child Abuse Investigator with the San Bernardino County Department of Social Services. I worked for Child Protective Services (CPS) for three years until I opened my private practice in 1984. CPS was the most demanding role in my Mental Health Practice History. My territory covered almost 10,000 square miles, and the Juvenile Court, where I adjudicated cases, was 70 miles from my office in Yucca Valley. The Morongo Basin communities embodied pent-up demand for CPS investigations in the early 1980s. The first mandatory suspected child abuse reporting law was passed in California in 1981.
Indeed, suspected child abuse reports poured in from School Principals and teachers, doctors' offices, public health nurses, attendance officers, extended family members, and neighbors. I worked without backup and was on call 24/7 the entire time. The distances I traveled between cases and the Juvenile Court and the overwhelming demand for investigations and case follow-ups made it necessary for me to become highly efficient. My requests for a vehicle and other tools were met with budget limitations and month-long delays.
Desperate to merge Mental Health and Child Welfare Practices, I commandeered a county vehicle from the County carpool. I charged a camera, dictaphone, and pager service to the county. I gathered files, forms, forms, and general stationary supplies. I taped photos of documents to the dashboard and sun visors so I could dictate while driving and turned the car's trunk into a file cabinet and storage closet. My unauthorized mobile office made this impossible job somewhat possible in this pre-cellphone era. I ignored or rejected requests and demands for completed forms that I never knew existed. I encouraged the bean counters to have me fired, which never happened. Though not appreciated by Social Service Administrators, my Maverick style was appreciated by the Morongo Basin professionals, attorneys, and judges in the Juvenile Court owing to my mobile responsiveness and practical Mental Health Practice approach to child welfare.
My only training day as a CPS investigator in San Bernardino did not prepare me for this job. Despite the lack of exercise, CPS expanded my learning experiences and increased the scope of my Mental Health Practice History. I learned investigative strategy from the detectives and deputy sheriffs with whom I shared cases. I acquired anatomical and medical knowledge from doctors and nurses who taught me to differentiate child abuse and neglect from childhood disease and injury. I became familiar with the heartbreak, and psychological trauma reporters experience witnessing child abuse and neglect. My Mental Health Practice skills helped me to embrace the ambivalence teachers, school administrators, family members, and neighbors experience when mandated or deciding to file suspected child abuse reports. I learned from judges, prosecutors, and defense attorneys how to prepare allegations and organize evidence to prove allegations to adjudicate cases. My Court reports became prototypes and facilitated change in the child welfare philosophy, especially in two areas: First involved moving from the idealistic reference of "Best Interest of the Child" to the pragmatic "Least Detrimental Alternative for the Child." Second, revising the concept of the "Non-Offending Parent" to the "Non-Protecting Parent."
The Marine Corps base in Twentynine Palms produced fascinating and frustrating jurisdictional issues in child welfare cases that challenged and enriched my Mental Health Practice. Judge Advocates, Naval Investigative Officers, Military Police, and Commanding Officers selectively exerted influence on the outcome of child abuse cases. In one case, a Commanding General (via his Staff Judge Advocates) threatened to close all the foster homes on base if I did not immediately remove an Officer's stepdaughter from her placement in an enlisted man's foster home.
Despite all my Mental Health, Social Work, and Child Welfare Ethics, I eventually backed down when ordered by the Director of Social Services, who said the County Board of Supervisors was taking too much pressure from the military.
Earlier that week, I placed the 13-year-old girl in the only available home with foster parents skilled in caring for teenage incest victims. This case was a powerfully sad reminder of how powerful people can disrupt appropriate Mental Health and Child Welfare Practices. Forty years later, I still feel appalled that undermining a pedophile officer’s command was more critical than the incest victims' condition and need for skilled care.
There were many foster homes in the Morongo Basin, but only a few were suitable placements for traumatized children or, in some cases, six distressed children from the same family. In the early 1980s, the foster home licensing process focused more on household conditions. The administration concluded that the number of licensed foster homes met the need for child welfare placements and thus declined to devote department resources to my concern for quality foster homes. My Mental Health Practice History assured me that I could not expect the Mental Health of abused children would improve if foster parents were not adequately vetted, trained, supported, and supervised. I felt compelled to address the problem myself.
A decade earlier, my Mental Health Practice History related to substance abuse developed the community organization and program development skills I applied to child welfare. I began a public awareness campaign on the need for Morongo Basin foster homes. I relied on print media, radio interviews, and public addresses to religious, fraternal, sororal, civic, and service organizations. With exceptional help from a few experienced and compassionate foster parents, we delivered a program that recruited, trained, and provided a support group for foster parents.
I began collaborating with interested therapists to develop treatment plans for children and parents where child removal was necessary and reunification was possible. I initiated training and clinical supervision for the few Baccalaureate level social workers in the Yucca Valley office to carry adjudicated child welfare cases. Eventually, I developed a Children’s Services Team. It seemed around every corner, unmet child welfare needs were crying out for attention. This fantastic job finally took its toll on my health. In 1984 I opened my private Mental Health Practice office in Yucca Valley and resigned from my position with the county later that year.
Private practice was never my goal. I chose the Social Work profession because I was committed to working with poverty. My options were limited: 1) Move my family again as we were still adjusting to our move from metropolitan New York 4 years ago; 2) Take a job in San Bernardino or Riverside, adding 3 hours of commuting time each day; or 3) Go into private practice. The latter choice, though risky, was best for my family. I feared private Mental Health Practice History would compromise my commitment to serving less fortunate folks. In 6 months, my practice was on its way to success, mainly due to my notoriety and reputation as the area’s child abuse investigator. I resolved my value dilemma by institutionalizing three principles: 1) Keep fees as low as possible and fee scale; 2) Offer pro bono service, where possible; and 3) Volunteer work in the community.
I enjoyed the scheduling flexibility that came with my private Mental Health Practice History, which made it easier to give back to the desert communities I had learned to call home. I organized a Child Abuse Task Force, trained at Parents United in San Jose, and developed a Child Sexual Abuse Treatment Program in the Morongo Basin. I volunteered to counsel residents of Unity Home (a shelter for abused women, men, and children). And I worked with Rotary International to develop youth service and foreign exchange programs. I spent a decade on the United Way Board of Directors, leading the annual fund drive and training volunteers, and served as president for three consecutive years. My United Way gavel was retired when I stepped down as president, and I received the 1994 Volunteer of The Year Award from the California State Legislature.
At the Morongo Unified School District (MUSD) request, I developed the Adolescent Substance Abuse Program (ASAP), a group counseling diversion program for students expelled from high school for possessing drugs or alcohol on campus. Scores of ASAP teens recovered self-esteem, experienced identity integration, and acquired sustainable resilience by developing skills to embrace and share feelings and manage emotions constructively while accumulating collective sober days. A few years later, MUSD asked me to design a pilot counseling program for elementary school students with academic and social adjustment problems. I developed protocol and implemented services for the “School-Based Counseling Program” (SBCP) at Yucca Valley Elementary School. I trained and supervised a clinical intern the following academic year to provide SBCP services in two MUSD elementary schools. My 1999 SBCP annual report became the prototype the California legislation used to create funding legislation for mental health services in public schools, which has continued for over two decades. MUSD invited me to develop an education program for incoming parents of 7th graders. I tested my long-held hypothesis that parenting education programs needed to increase focus on the parenting experience as we discussed the developmental needs of children. I also served three years as a consultant (counselor and program developer) to San Bernardino's County Community School Program, which educated 7th to 12th graders expelled from the MUSD. My Mental Health Practice History owes much to the New York and California public school systems for affording creative opportunities to improve the mental health of children, adolescents, and parents.
Private Mental Health Practice allowed me to return to my other professional passions, teaching and lecturing about: "Educating Your Mental Health." I taught graduate and undergraduate courses as an adjunct psychology, sociology, and education instructor for Chapman College and National University. I taught sociology at the College of the Desert (COD) and Copper Mountain College (CMC). I was a frequent guest lecturer at CMC, COD, several California State University campuses, Loma Linda University, Redlands Community College, and the University of Redlands.
In 1988 My Mental Health Practice history earned admitting privileges at Canyon Springs Hospital in Palm Springs, CA, where I worked with several psychiatrists. In the early 1990s, I partnered with A.J. Botwin, MD (psychiatrist), to develop the Desert Psychotherapy Institute (DPI). This psychiatric and psychotherapy facility provided fee-scaled services to patients and training for students and interns. DPI offered audio/visual recording tools and reciprocal mirrors for supervision and training. As the Clinical Director of DPI: 1) I became a consultant/liaison for Las Encinas Hospital's in-patient programs. 2) I served as a field instructor for social work students attending CSU at San Bernardino and Loma Linda University 3) At CalState Fresno, I assisted in the curriculum development of the "Essentials of Emergency Response Program." Then I traveled the state teaching this federally funded mandatory program to every child abuse investigator in California.
Beginning in the 1990s and for two decades, I contracted with the San Bernardino County Department of Social Services to provide psychotherapy to children and families with Juvenile Court dependency cases. I developed clinical strategies for reunification therapy and collaborative protocols with CPS staff. My Mental Health Practice History led to a request from the California Superior Court to develop a child custody mediation program for the Morongo Basin. My mediation model was based on securing agreements first in legal custody matters owing to its education and inclusive and cooperative communication processes. These achieved agreements encourage parental trust in their legal rights and increase their motivation to challenge the more complex areas of physical custody, visitation, travel, step-families, and dispute resolution. My custody mediation model also enhanced parental responsiveness to their children’s needs and rights by utilizing a psychodrama method: I spoke to parents from the child(ren) perspective, directly addressing them as mom and dad. By 2010 I settled back to a less diversified clinical practice with individuals, couples, and families and periodic clinical supervision of interns.
2021 was my chosen year for retirement from clinical practice. I stopped taking new patients that year and continued reducing my clinical hours within each patient’s comfort zone. My post-retirement goals include developing and enriching this website, "Educate Your Mental Health," with writings based on my Mental Health Practice HIstory. My goals are to assist the general public in knowing Educating Your Mental Health is a feasible, cost-effective, and sustainable way to be healthy. To help mental health practitioners learn practical methods that teach their patients to develop wise consciousness and healthy habits. And to influence social policy analysts and architects to focus on preventing mental illness by promoting mental health education and addressing the underlying social ills that cause mental illness.
Throughout my Mental Health Practice History I have paid homage to Newton’s metaphor by seeking out the giants (a partial list below) in the fields of Psychoanalysis, Psychiatry, Psychology, Neuropsychology, Social Work, Sociology, Education, and Systems and Organization theory and practice. Indeed, I climbed on their shoulders and enjoyed working with some, trained with others, and learned from them all and the ancestral masters whose shoulders they stood upon.
